The Myth of “Evidence-Based” Treatment of Depression
In a blog post at the end of April, Thomas Insel, Director of the National Institute of Mental Health (NIMH), came out with a long overdue critique of the “bible” of diagnosis of mental disorders, the DSM (Diagnostic and Statistical Manual of Mental Disorders). Inspired by the publication of the new DSM-V, revised since publication of the DSM-IV-TR, Insel described how DSM diagnoses fail to make sense; the “criteria” in various diagnoses are often the same, across diagnoses. Further, the DSM formal diagnoses rarely inform clinicians about the source of a problem, or the best “treatment.”
The NIMH leader suggests the importance of studying brain circuits in etiology and treatment for mental disorders, despite protestations by some mental health care providers who have a knee-jerk, anti-biology bias. Almost a decade ago our own research team began questioning why, in many studies comparing medication to various kinds of talk psychotherapy, findings appeared to demonstrate that treating depression (the most commonly studied disorder) with medications had results equivalent to or less effective than talk therapy alone. Many psychotherapy outcome studies have been aimed at the turf wars between different brands of talk-focused psychotherapy: CBT (cognitive behavioral treatment); ACT (Acceptance and Commitment therapy); IPT (Interpersonal Psychotherapy); and “psychodynamic” treatment. However, the studies that seemed most off base, based on clinical experience, were those concluding that “talk therapy” was as good or better than treatment with medication or some combination of treatments.
As a clinical and research psychologist, I see clients (or patients, however you prefer to refer to the people clinicians see for psychological services) and hear about many of them from my doctoral seminar students and from other psychotherapists for whom I’m a consultant. Many patients I see and/or hear about, need medication in addition to psychotherapy –no matter what the brand of “talk therapy” employed.
In my practice I make use of techniques from many modes of talk psychotherapy –what I do in collaboration with patients is highly “case specific” and I need all the tools possible in my tool box of interventions. I am first and foremost “a pragmatist;” see what works and don’t stop trying until something works. Furthermore, not infrequently, patients don’t make much headway in an active talk therapy treatment, regardless of the “type” or “techniques” used, until the most pressing symptoms have been somewhat reduced by appropriate medications. So I commonly make referrals to psychiatrists or general medical practitioners who hopefully know something about psychopharmacological treatment. But then how to explain the contradictory research, claiming that talk therapy is as good or better than psychopharmacological interventions.
All research is, bottom line, a story; the patriarchal and often snobby research establishment likes people to think that research is too difficult for “ordinary” psychologists or physicians, (especially women but also men); it’s too esoteric, a realm of activity reserved only for the most esteemed (even brilliant) characters. But down in the trenches, where we actually do research, it’s just a story. That goes for each and every project. Reflecting upon my anecdotal data, i.e. direct experience with patients, one at a time, I suspected that something was wrong with the prior studies ostensibly demonstrating that medicine was no better that ordinary talk therapy. I’m lucky, I work with a research team, and we set out to find out what was wrong with the going outcome research story.
Around 2002 I read a book first authored by psychopharmacologist Tom Lewis, “A general theory of love.” I liked Lewis’ thinking, met him at a psychotherapy research meeting and soon began sending him my patients who needed medications –particularly those who needed a real expert figuring out what medication they needed, in order to make optimal progress. I sent him “difficult cases,” people who had already tried this or that medication, prescribed by a less skilled psychiatrist or uninformed internist, that failed to reduce their symptoms. Many patients today are prescribed medications by internists or general practitioners who have had little or no special training in mental disorders. In some states psychologists are being trained to prescribe psychoactive medicines, but in most, we don’t. If we’re seeing people we think need medicine we refer them to a psychiatrist. However in most cases, psychologists (or other mental health professionals) are not even seeing the patients at all. Most people suffering from anxiety and/or depression (for example) go to their general or family physician, explain that they’re anxious and/or depressed, and ask for an anti-anxiety and/or antidepressant medicine, not infrequently something they’ve seen advertised on TV, or something one of their friends is taking. The physician then prescribes the most currently popular medicine for what their patients tell them they’re suffering from. Contemporary patients generally know their own diagnoses; from research on the Internet, they’ve figured it out, and they’re usually correct. When a patient says, for example: “I’m depressed” the internist is most likely to prescribe an SSRI (selective serotonin reuptake blocker), assuming this is the best thing to do. And in many or even most cases, this is what the patient requests, again because of popular opinion. Sometimes it works, but too often it doesn’t and patients get discouraged. General physicians may add yet another “most popular” medicine. This is, however, all happening in the blind so to speak.
Neurotransmitter Circuits in Depression
So when we got suspicious about the comparative research concluding that medicine was no better than talk therapy, and furthermore, unlike medications, it ostensibly comes with no unpleasant side effects, we set out to tackle this mystery; why were studies supporting conclusions that were so counter to our own experience with numerous people. We turned to Tom Lewis. I had seen how he asked my referrals rather detailed though ordinary questions as he tried to ascertain what might work with particular patients. My colleague Jack Berry and I met with Lewis. We had a plan. We wanted to capture those questions in order to develop a measure that indirectly mapped on to something biological, something that allowed Lewis to decide what medication to try first. He was often right. We couldn’t “diagnose” or determine specifics by way of a blood test or even an MRI; we still can’t. We had seen –again anecdotally– that some people suffering from symptoms of depression (according to the criteria laid out in the DSM) responded to an SSRI, and others seemed to do better with a dopamine-related medication (for example Wellbutrin or Ritalin or an amphetamine.) Some seemed to respond best to both in combination.
These different patients didn’t fall into the old “categories” of different forms of depression, those who worry most about their relationships, or those who wake up depressed etc.; the differences that informed Lewis were how patients responded to simple questions, some of which are found on personality-type measures, or other ordinary life-preferences kinds of questions –“Do you get more parking tickets than other people?;” “Do you balance your checkbook regularly?;” “Does your mind tend to wander when listening to others in conversations?” None of the questions were particularly odd, none made patients feel “crazy.” But responses to these simple questions informed Lewis, and other experienced psychiatrists or psychopharmacologists what kind of medicine was most likely to help a particular patient.
The three of us captured all the questions Lewis could remember asking of new patients. We got additional questions from patients I’d sent to see Lewis. The list grew. Finally we had our measure and we began to pilot it, trying it out on different groups of “normal” or mostly normal people, the usual student population. We checked out how the items worked, asking: Did the questions that indicated a patient was likely to need a serotonergic agonist (a drug that increases the availability of serotonin) hang together or form a coherent subscale. Did the questions indicating that someone might need a drug that increased levels of dopamine hold together? They did. We had our subscales, and the items –that is each individual question—were reliable. We were ready for our bigger study, in which we tried to validate these two subscales, simply referred to as “Low-Serotonin” and “Low Dopamine” were reliably associated with people who suffered from mental disorders that we knew were best treated by either a dopamine-related medicine or a serotonin-related medicine. For example, we knew that attention deficit and hyperactivity disorder is often successfully treated with Ritalin, a medicine that increases dopamine, or dopaminergic agonist. In contrast, obsessive-compulsive disorder is usually best treated by drugs that increase serotonin, serotonergic agonists, the most famous of which is Prozac, and then all the similar drugs that have followed. The children and grandchildren of Prozac.
We collected data anonymously online, using already known measures of ADHD, depression, and OCD. We asked participants to fill out a series of measures including a standard measure of depression, a measure of “Generalized Anxious Temperament” (associated with anxiety), a screening measure for ADHD and another indicating OCD, along with our new measure that we titled the “Neurotransmitter Attributes Questionnaire,” the NAQ. We also asked them to indicate if they suffered from any mental disorder, and if so, what. We asked if they were prescribed one or more psychiatric medicine, and if so, what medicines. Our results indicated that our subscales of “Low Dopamine” and “Low Serotonin” were valid. Participants who scored high on the ADHD screening scale, also rated high on the Low Dopamine subscale. Those who were high on OCD were also high on the “Low Serotonin” subscale.
Then we looked at the most interesting and perhaps important question –how would people who were high on the standard measure of depression used in the study, look on the “Low Serotonin” and “Low Dopamine” sub-scales. As we suspected from clinical experience, mirrored by Lewis and other psychopharmacology experts, the ordinary protocol for treating depression with an SSRI was not always likely to be successful. Some participants who were high in depression needed one type of medicine (they rated high on the Low Serotonin subscale) and some needed another (they rated high on the Low Dopamine subscale). Still others needed both; they were high on the depression scale and high on both of our subscales. The study demonstrated what experienced psychopharmacologists and general psychiatrists (or most of them), already know. It is important to carefully interview new patients, ask them a series of simple questions, and intuit from their responses, what medication is most likely to be effective. What our measure did was take that ostensibly intuitive piece and transform it into a measure that could be used by relatively untrained MDs or prescribing physician assistants and nurse practitioners, or psychologists whenever, wherever, we manage to gain prescription privileges.
Perhaps more important, the NAQ and the study in which we used it –and we’re still collecting data anonymously, online (if anyone wants to participate in this anonymous online study, just follow this link), may throw a long-deserved wet blanket on the famous and misleading “outcome studies,” specifically for depression. These outcome studies have had a huge impact, for example in England there has been a move to use CBT alone. In the U.S. (and perhaps world-wide) the press had had an anti-medication hey-day over studies ostensibly proving that CBT (along with several other treatment modalities) is as good as medication. The war on medications has had a serious impact on patients; they’ve become afraid to use medicine. When they’re told that research had confirmed that CBT (for example) works just as well or better that treatment with medicine, without any of those frightening potential side-effects, patients refuse to take medicines.
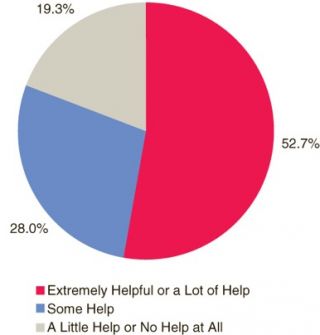
SSRIs don’t work in all cases of depression
There’s an inherent problem with all these famous outcome studies. In every study, only ONE class of medicine has been used. In almost all, the medications have been serotonergic agonists. But as psychopharm experts have long known, and as the NAQ demonstrates, at least a third of depressed patients need a dopaminergic agonist. So of course the studies comparing CBT to pharmacological treatment of depression “proved” that CBT was as good or even better than psychopharm treatment, given that at least one third of the depressed research subjects were being given the WRONG kind of medicine. There is no way to say that CBT is “better” than medicine, if participants are being given the wrong medicine. The whole comparison becomes ridiculous.
The results of our study, published by SAGEOpen, “Personality, Psychopathology, and the Neurotransmitter Attributes Qeuesionnaire, are free for all to download and review.
So much for “evidence-based” mental health care. This popular myth is resting upon erroneous studies, in which everyone is given the same class of psychiatric medicine, working on the same brain or neurotransmitter circuits. But not everyone needs the same class of psychiatric medicine. Not everyone suffering from depression or anxiety needs the same class of medication. The idea that we have substantial evidence in mental health treatment has to be questioned and for the most part, discarded. We don’t have evidence-based treatment for depression, not yet; we have not yet conducted reasonable, appropriate, sensible research upon which to decide what is effective. Medications need to be prescribed case-specifically, and I would add here, so does the modality of talk-based psychotherapy.